[Publication] How have hospitals adapted their infrastructure during the COVID pandemic? A scoping literature review

Source: pixabay
Authors of the summary: Costase Ndayishimiye, Katarzyna Dubas-Jakóbczyk
The COVID-19 pandemic has put unprecedented pressure on the hospital sector all over the world. This showed the importance of preparing and planning for the future in the event of an outbreak that would overwhelm all aspects of hospital operations on a rapidly expanding scale. Our main goal was to identify, map, and systemize the literature on the relationships between the COVID-19 pandemic and hospital infrastructure adaptation and capacity planning around the world. We conducted a systematic scoping review of the literature following the six steps of the Teare and Taks (2020) methodological guidelines (1). We searched the Web of Science, Scopus, and PubMed databases and hand-searched English-language publications published between December 2019 and December 2021.
Main results
A total of 106 papers were included in the review: 102 empirical studies and four technical reports. Empirical studies entailed five reviews, 40 studies focusing on hospital infrastructure adaptation and planning during the pandemics, and 57 studies on modelling the required hospital capacity, measured primarily by the number of beds. Most studies were conducted in high-income countries and published within the first year of the pandemic.
The strategies adopted by hospitals could be classified into short-term and long-term. The former were designed to lessen immediate pressures on hospitals during the pandemic, but they were not meant to last beyond it. Long-term strategies are the opposite of a quick fix and are integral to planning hospital infrastructure for the future. In addition to these strategies dealing exclusively with hospital infrastructure, other concurrent and complementary activities were also needed in response to COVID-19 crisis management. For example, hospital capacity needs were projected; non-urgent procedures were cancelled; patients were transferred within or out of hospital networks; and intensive care unit (ICU) surge guidelines were adjusted (Fig 1).
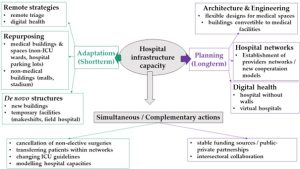
Fig 1. Hospital infrastructure adaptation and planning strategies during the COVID-19 pandemic. Source: Ndayishimiye et al. (2022).
Short-term hospital Infrastructure adaptation mechanisms
Short-term adaptations aimed at quickly expanding hospital infrastructure capacity. They can be categorised into three broad groups: (a) repurposing medical and non-medical buildings; (b) establishment of de novo structures; and (c) remote adjustments.
Medical facilities were partially or completely repurposed. The conversion of medical facilities also included using their spaces and annexes, such as turning a hospital parking lot into a treatment facility (2). Attempting to satisfy the demand for beds also meant identifying existing non-medical buildings that might be suitable for use. Training halls, exhibition centres, malls, and schools, among other things, have been set up to temporarily relieve pressure on hospitals. Quite often, when converting non-medical buildings into medical structures, new structures were also erected, such as tents.
The evidence suggests that the strategies have varied depending on pandemic wave, level of urbanization and the availability of convertible spaces (3). Temporary facilities display chief features, making them crucial to managing rapidly growing outbreaks like COVID-19 (4). When converted to hospitals, large public venues, such as stadiums, result in a significant boost in terms of capacity (beds, space, etc.). For instance, the London NHS Nightingale has established the equivalent of 54 district general hospitals in terms of bed capacity within only two weeks (5). Transforming public spaces into care facilities eliminates the need for costly new physical infrastructure and investment costs. Because fewer nurses and doctors are needed than in typical hospitals, and since most cases require standard procedures, the operating costs are seemingly lower. Once the outbreak has passed, the converted facilities can be reconverted to their original functions, preventing inefficient long-term space utilization. This is especially important in highly populated areas. At the same time, however, temporary facilities could serve only patients with mild to moderate symptoms and perform a few set activities, such as triage and speedy referral. Research (6) claims that temporary facilities, regardless of their purpose, fall short of typical hospital requirements. Many converted buildings’ heating systems, ventilation, and air conditioning systems are incapable of recreating a regular hospital’s intensive care (ICU) beds.
Long-term hospital infrastructure planning
Three sorts of long-term strategies are (i) architectural and engineering changes, (ii) hospital networks, and (iii) digital approaches. For the former, research indicates that many current buildings have difficulty adjusting because of their inflexible and challenging-to-change designs. Hospitals are built for highly specialized medical purposes, which is often at odds with the necessity to expand capacity that can accommodate evolving and changing circumstances over time (7). This exemplifies how architectural design methods influence a building’s capacity to adapt. Future medical structures and their annex buildings will need to be flexible in their designs to allow for a variety of modifications to critical healthcare facilities, with a full spectrum of emergency unit capabilities (e.g., modular, demountable walls, parking lots equipped with in-hospital installations).
As no hospital alone is able to provide sufficient response during the pandemic, the need for strengthening providers networks has been highlighted during COVID-19. Patients were moved between the hospital networks (8) and even to unaffiliated private hospital providers (9). To ensure a successful response to future health emergencies and an overall increase in the resilience of health systems, it is essential to strengthen collaboration across different stakeholders, including providers, payers, and decision makers.
Diverse digital solutions may be applicable in the short and long terms. They can significantly assist physical hospitals by operating virtual hospitals and clinics that provide a range of remote and outpatient services (10,11). With regard to remote triage and infection detection, the COVID-19 pandemic gave rise to a number of innovations (12). If explored further, these technologies could assist hospitals in making future plans for proper infection control, either by lowering nosocomial infections (i.e., infections that originate in hospitals) in high-risk hospital departments or by enhancing hospital preparedness for future infectious outbreaks. Additionally, adopting smart devices to care for chronic conditions linked to the elderly would be beneficial in offloading hospitals from the aging population (10). Furthermore, thanks to digital/remote solutions, the patient’s stay in a clinic or hospital would no longer be the exclusive source of useful data for care and research purposes.
Conclusions
The hospital sector adopted diverse strategies to adjust its infrastructure during the COVID-19 pandemic. Temporary facilities are indispensable to help minimize negative outcomes when hospitals require more capacity by performing essential functions such as triage, isolation, sheltering, and rapid transfer. However, there are limitations that prevent them from being the same as regular hospitals (e.g., difficulties in heating, ventilation, and air conditioning systems). For long-term solutions, these limitations should be addressed. Flexible designs, adaptable structures, and hospital annexes that can be easily adapted to serve as medical facilities are needed. System-level changes, such as new architectural guidelines, more hospital networks, and strengthened public-private partnerships (PPPs), as well as exploring digital technology opportunities, are needed if we are to respond properly to future rapidly growing outbreaks.
Full text article: Ndayishimiye C, Sowada C, Dyjach P, Stasiak A, Middleton J, Lopes H, Dubas-Jakóbczyk K. Associations between the COVID-19 Pandemic and Hospital Infrastructure Adaptation and Planning—A Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(13):8195.
Disclaimer: The article, whose summary is presented here, is an excerpt from a thesis submitted to the Institute of Public Health of Jagiellonian University to fulfil the requirements for the award of the Master degree in European Public Health with a specialization in the Governance of Health Systems in Transition, academic year 2021/2022 (run with the support of the Erasmus+ programme of the European Commission). The thesis was written by Costase Ndayishimiye and supervised by Katarzyna Dubas-Jakóbczyk.
Blog Zdrowia Publicznego, red. M. Zabdyr-Jamróz, Instytut Zdrowia Publicznego UJ CM, Kraków: 22 lipca 2022
References:
- Teare G, Taks M. Extending the scoping review framework: a guide for interdisciplinary researchers. Int J Soc Res Methodol. 2020;23(3):311–5.
- Louri NA, Alkhan JA, Isa HH, Asad Y, Alsharooqi A, Alomari KA, et al. Establishing a 130-Bed Field Intensive Care Unit to Prepare for COVID-19 in 7 Days in Bahrain Military Hospital. Disaster Med Public Health Prep. 2021;15(1):e34–43.
- Iftimie S, Lopez-Azcona AF, Vallverdu I, Hernandez-Flix S, De Febrer G, Parra S, et al. First and second waves of coronavirus disease-19: A comparative study in hospitalized patients in Reus, Spain. PLoS One. 2021;16(3):e0248029.
- Chen S, Zhang Z, Yang J, Wang J, Zhai X, Bärnighausen T, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305–14.
- Oliver D. David Oliver: Were Nightingale units and fever hospitals ever workable responses to covid-19? BMJ. 2021;374:10–1.
- Webster C, Wordsworth M, Marsden M, Navaratne L, Bowley D, Chaloner E, et al. C4: ‘Command, control, coordination and communication’ at NHS Nightingale, London: introducing the tactical commander. J R Soc Med. 2020;113(8):299–301.
- HSU J. How the Covid-19 Pandemic May Reshape U.S. Hospital Design [Internet]. New York City; 2020 [cited 2022 Feb 11]. Available from: https://undark.org/2020/04/16/covid-19-modified-hospital-design/
- Budhiraja S, Indrayan A, Aggarwal M, Jha V, Jain D, Tarai B, et al. Differentials in the characteristics of COVID-19 cases in Wave-1 and Wave-2 admitted to a network of hospitals in North India. medRxiv. 2021;1:1–18.
- Illman J. NHS block books almost all private hospital sector capacity to fight covid-19 [Internet]. Policy and Regulation. 2020 [cited 2022 Mar 22]. Available from: https://www.hsj.co.uk/policy-and-regulation/nhs-block-books-almost-all-private-hospital-sector-capacity-to-fight-covid-19/7027196.article
- Mannix L. Australia’s first virtual hospital rolls out for COVID-19 patients [Internet]. The Sydney Morning Herald. 2020 [cited 2021 Mar 16]. Available from: https://www.smh.com.au/national/australia-s-first-virtual-hospital-rolls-out-for-covid-19-patients-20200329-p54ezj.html
- Headley M. Hospitals and health systems adapt to fight COVID-19 [Internet]. ASHE Health Facilities Management. 2020 [cited 2021 Mar 15]. Available from: https://www.hfmmagazine.com/
- Mageit S. Doccla and Northampton NHS trust trial virtual wards for vulnerable patients. EMEA Digital Health [Internet]. 2020; Available from: https://www.mobihealthnews.com/news/emea/doccla-and-northampton-nhs-trust-trial-virtual-wards-vulnerable-patients
 FACEBOOK
FACEBOOK INSTAGRAM
INSTAGRAM X
X LINKEDIN
LINKEDIN YOUTUBE
YOUTUBE